Life expectancy is a measurement that summarizes almost everything about quality of life in a society, and therefore even tiny increases or decreases are indications of profound changes with deep consequences. In a somewhat shocking discovery, life expectancy declined overall in the United States by 0.1 year from 2014 to 2015, according to the Centers for Disease Control and Prevention (CDC), the federal government agency responsible for compiling and analyzing the relevant statistics. This is the first overall decline for the entire population since 1993, at the height of the AIDS epidemic.
From 2014 to 2015, life expectancy at birth declined for the entire population to 78.8 years, a decrease of 0.1 year; for males to 76.3 years, a decrease of 0.2 years; for females to 81.2 years, a decrease of 0.1 year.
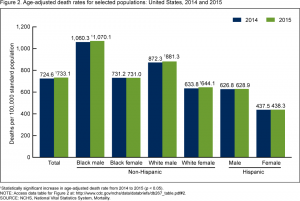
The decline in life expectancy and corresponding increase in death rates is best understood as the culmination of negative trends within certain subpopulations, particularly non-Hispanic whites. According to the CDC report cited, the age-adjusted death rate for the total population increased 1.2% from 2014 to 2015, but for non-Hispanic white females by 1.6%, for non-Hispanic white males by 1.0%, and for non-Hispanic black males by 0.9%. There was no significant change for non-Hispanic black females, Hispanic males or Hispanic females.
Life expectancies for non-Hispanic whites were flat in both 2012 and 2013 but declined in 2014, according to a 2015 paper published on PNAS, but offsetting increases among Hispanics and non-Hispanic blacks prevented the overall average from falling. “The midlife mortality reversal was confined to white non-Hispanics; black non-Hispanics and Hispanics at midlife, and those aged 65 and above in every racial and ethnic group, continued to see mortality rates fall. This increase for whites was largely accounted for by increasing death rates from drug and alcohol poisonings, suicide, and chronic liver diseases and cirrhosis.”
Disparities correlated with education and race have long been noted, so the data could be viewed as a convergence. A 2012 article in Health Affairs reported that, as of 2008, “US adult men and women with fewer than 12 years of education had life expectancies not much better than those of all adults in the 1950s and 1960s … [and] white US men and women with 16 years or more of schooling had life expectancies far greater than black Americans with fewer than 12 years of education — 14.2 years more for white men than black men, and 10.3 years more for white women than black women.”
Attempts to identify geographic disparities in death rates have encountered serious statistical difficulties, but generally have found wide but consistent variations. A recent study published in the Journal of the American Medical Association in December 2016 observed, “Geographic regions with elevated mortality rates differed among causes: for example, cardiovascular disease mortality tended to be highest along the southern half of the Mississippi River, while mortality rates from self-harm and interpersonal violence were elevated in southwestern counties, and mortality rates from chronic respiratory disease were highest in counties in eastern Kentucky and western West Virginia.”
Death rates in the United States have been in a very long, steady decline, and a 2015 article in the Journal of the American Medical Association described remarkable reductions (age-adjusted) between 1969 and 2013: 42.9% from all causes, 77.0% from stroke, 67.5% from heart disease, 39.8% from unintentional injuries, 17.9% from cancer and 16.5% from diabetes. However, after 2010 (through 2013, the last year of the study), death rates stopped declining and were essentially flat.
In an internal interview, Dr. Jiaquan Xu of the CDC said, “For the total US population, life expectancy decreased … mainly because of increases in mortality from the 13 causes of death among the 15 leading causes of death, such as heart disease, chronic lower respiratory disease, unintentional injuries, stroke, Alzheimer’s disease, diabetes, kidney disease, suicide, septicemia, chronic liver disease, hypertension, Parkinson’s disease and pneumonitis due to solids and liquids.” By comparison, “We haven’t seen the increase in mortality from so many leading causes of death for a long time. The age-adjusted death rates increased significantly for three of 10 leading causes of death in 2014, two in 2013, one in 2012 and five in 2011. It is an unusual year. Again we don’t know why.” However, Dr. Xu said, “We don’t think we have reached a peak in life expectancy…. We also don’t know if the increase in mortality in 2015 will continue in 2016…. But it is too early to say that the mortality in 2016 will go down or continue going up. We will see what happens when the 2016 final file is available.”
More Posts by The Author:
Heavy Rain, High Winds, Flooding Wed–Thu: Advisory for wind, watches for inland and coastal flooding posted
River Flood Warnings in RI, MA, CT: Wed through Fri, streets may be impassable at times
Snow possible but unlikely Sat mid-day: Little accumulation likely
Snow Thu Night: One inch expected
Significant Snow Storm Tue 5am – 3pm: Likely 6in but remote possibility up to 18in


