News Analysis
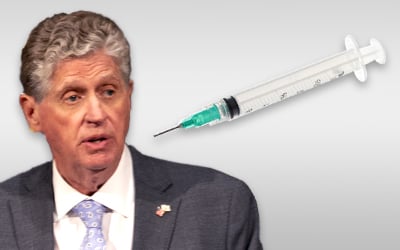
Will RI Governor Dan McKee stand his ground on the August 18 mandate that all RI health care workers must receive their final dose of COVID-19 vaccine by October 1 or face consequences, possibly including termination of employment?
There has been considerable resistance, including a letter drafted by Rep. Arthur Corvese signed by 32 members of the state House of Representatives, “respectfully calling upon Governor Daniel McKee to amend the October 1st deadline… and to direct the Rhode Island Department of Health to develop appropriate guidelines for those individuals to retain their employment while maintaining the public health.” (Rep. Raymond Hull removed his name this morning, according to the Legislative Press and Information Bureau.)
The governor has shown a reluctance to expend political capital in such disputes, dissembling for two full weeks on requiring masks in schools. During that time, he declined to issue a state mandate while also saying that he expected local school districts to comply with guidance from the US Centers for Disease Control and Prevention (CDC) – which recommends “universal indoor masking” – until ultimately reversing himself and issuing Executive Order 21-87 on August 19. During those two weeks, the governor allowed local school committees and superintendents to fight it out separately with parents and trade labor unions.
Who is resisting nationally?
It is well established that vaccination take-up varies enormously depending upon such factors as education and location.
A study published July 30 by the CDC in their flagship journal Morbidity and Mortality Weekly Report noted that, “Vaccination coverage was highest among physicians and advanced practice providers (75.1%) and lowest among nurses (56.7%) and aides (45.6%). Among aides (including certified nursing assistants, nurse aides, medication aides, and medication assistants), coverage was lower in facilities located in zip code areas with higher social vulnerability (social and structural factors associated with adverse health outcomes), corresponding to vaccination disparities present in the wider community.”
Furthermore, the study said, “The proportion of persons who declined COVID-19 vaccination ranged from 11.1% among physicians to 33.2% among aides. Reported recent COVID-19 infections ranged from 0.7% among physicians to 3.0% among aides. The percentage of aides who were completely vaccinated was lower among those working in facilities located in ZIP code areas with higher proportions of ethnic and racial minorities (43.5% versus 50.5%), lower household median income (40.5% versus 48.1%), higher poverty (42.4% versus 49.2%), and lower high school completion (42.2% versus 49.3%).”
Why is there any reluctance among health care professionals to be vaccinated, as the overwhelming scientific consensus is that COVID-19 vaccines authorized in the US are safe and effective? The American College of Obstetricians and Gynecologists “recommends that all eligible persons, including pregnant and lactating individuals, receive a COVID-19 vaccine or vaccine series,” countering a frequent objection cited as a basis for hesitancy.
Legal structure for the mandate
Technically, the Rhode Island health care worker vaccination mandate was not issued by the governor but by the RI Department of Health (RIDOH) as a formal emergency rule. RIDOH explains, “The regulation applies to all individuals who work in RIDOH-licensed health care facilities and all licensed healthcare providers, whether they work in a licensed facility or not. ‘Healthcare worker’ means any person who is temporarily or permanently employed by or at, or who serves as a volunteer in, or has an employment contract with, a RIDOH-licensed healthcare facility, and has or may have direct contact with a patient in that health care facility. ‘Healthcare provider’ means any person licensed by RIDOH to provide or otherwise lawfully providing health care services.”
DOH minced no words in their justification for the emergency regulation: “The novel coronavirus SARS-CoV-2, also known as COVID-19, has mutated into a more contagious variant, known as the Delta variant. As of July 4, 2021, Rhode Island had a ‘moderate transmission’ rate of 11.2 cases per 100,000 people, but as of August 17, 2021, Rhode Island’s transmission rate has increased to ‘high transmission’ of more than 187 cases per 100,000 people. New hospitalizations by week have more than quadrupled within that same time period.”
The regulated class presents an especially dangerous threat to the public, DOH said: “Health care workers and health care providers interact with some of Rhode Island’s most vulnerable populations: individuals who are immunocompromised and individuals with co-morbidities. These vulnerable populations are at risk for adverse health outcomes from COVID-19. As COVID-19 positive individuals are often asymptomatic or presymptomatic, health care workers and health care providers may unintentionally spread infection to these vulnerable patients. In order to protect these vulnerable populations, RIDOH is mandating that all health care workers and health care providers be vaccinated against COVID-19 by October 1, 2021.”
The broad scope of the DOH definition of “health care worker” appears to encompass everything from pharmacy aides to emergency medical technicians (EMTs) on ambulances, but this is reasonable given that they are likely to encounter precisely the vulnerable patient population at greatest risk from complications of COVID-19 if infected. It is relatively common for firefighters and police officers to hold EMT certification, leading to claims that a vaccine mandate is a violation of collective bargaining agreements and consequent threat of lawsuits by trade labor unions, but it is difficult to imagine a court giving much credence to such objections.
Reading between the lines, it seems clear that the governor is pressed between opposing forces: the doctors and scientists on one side, and the politicians and unions on the opposite side. The governor could tell DOH to reverse the vaccination mandate, but that could have major fallout, even protest resignations from senior staff, if he tried it. DOH has made clear in the course of their formal rulemaking that they are strongly committed to the mandate.
So far, Gov. McKee has exhibited one great management strength: he knows what he doesn’t know – he takes advice on medical matters from doctors and DOH, and he takes advice on hurricane planning from emergency management experts and the National Guard. There is no legitimate reason for the governor to back down on the vaccination mandate for health care workers, just as there is no legitimate reason for the vast majority of health care workers to refuse vaccination.
More Posts by The Author:
Heavy Rain, High Winds, Flooding Wed–Thu: Advisory for wind, watches for inland and coastal flooding posted
River Flood Warnings in RI, MA, CT: Wed through Fri, streets may be impassable at times
Snow possible but unlikely Sat mid-day: Little accumulation likely
Snow Thu Night: One inch expected
Significant Snow Storm Tue 5am – 3pm: Likely 6in but remote possibility up to 18in


