Only 2.2% of Rhode Island residents have antibodies in their blood, known as “sero-prevalence,” against SARS-CoV-2, the virus that causes COVID-19, Brown University Professor Philip Chan, MD, the consultant medical director for the Division of Preparedness, Response, Infectious Disease, and EMS at the RI Department of Health (RIDoH), announced this morning on a press conference call. This result was much lower than expected, from a carefully designed study in May that invited 5,000 randomly selected households to be tested for free and of which about 10% accepted the offer, resulting in tests on 1,032 individuals of whom 24 were positive for antibodies.
Unlike the conventional nasal-pharyngeal swab PCR tests used to detect active infection, antibodies develop several weeks after infection: A positive sero-prevalance test means that someone had COVID-19 in the past, even if they were not aware of it or had only mild symptoms, and has recovered. The test for antibodies has a specificity (probability that a negative result is correct) of 99.6% and a sensitivity (probability that a positive result is correct) of 88%.
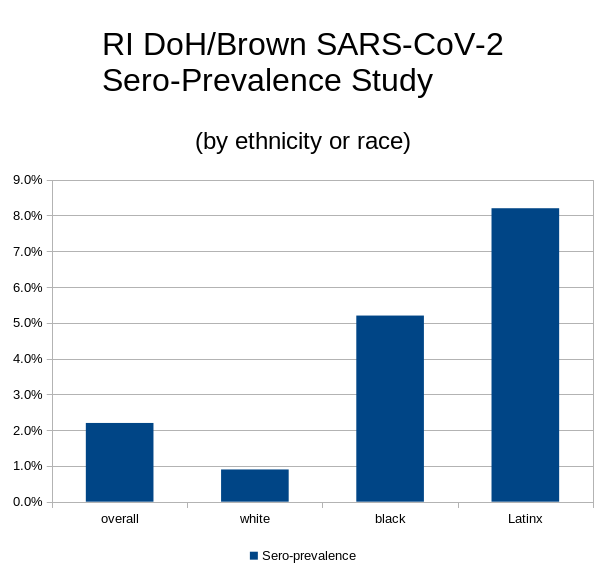
An important finding was that sero-prevalence among African American and Latinx test subjects was disproportionately higher than among white people, mirroring the findings of PCR tests. Chan said that the statistical team was able to provide a high degree of sampling accuracy, with a 99% confidence interval (CI) that the overall prevalence, estimated at 2.2%, is no less than 1.0% and no greater than 3.9%. For Latinx test subjects, the estimated sero-prevalance is 8.2% (3.7x the general population), with a 99% CI between 3.4% and 15.8%. For African American test subjects, the estimated sero-prevalence is 5.2% (2.4x the general population), with a 99% CI between 0.3% and 18.7%. For white test subjects, the estimated sero-prevalence is 0.9% (0.4x the general population), with a 99% CI between 0.1% and 2.4%.
The widely varying CI for different sub-populations is a consequence of a smaller number of test subjects, increasing the sampling uncertainty. However, the ethnic and racial differences were, according to Chan, deemed statistically significant. Differences by sex or gender did not appear to be statistically significant, he said.
While it remains unknown whether the presence of antibodies confers any immunity to the virus and if so to what extent, the main take-away from the study is that the remainder of the population, 97.8%, certainly are still vulnerable to infection. The good news is that containment measures – staying at home if sick, wearing face coverings, maintaining physical distance, washing hands frequently, and so on – have been very effective in limiting community spread of the virus, accounting for the unexpectedly low prevalence. The bad news is that such containment measures will have to be maintained for the foreseeable future, even as businesses and the economy reopen.
The study, a collaboration by RIDoH and Brown, puts RI in a position of world leadership in understanding the epidemiology of the new virus. While similar studies have been done in limited sub-populations inside and outside the US, this is the first scientifically rigorous assessment of sero-prevalence in a large general population such as an entire state. Guidance from it will drive public policy decisions, not only within RI but likely nationally and possibly even internationally. RI is the national leader among the states in testing, having completed PCR tests on approximately 40% of the population and, as of last week, conducting 4,500 tests in a single day.
