Jeff Zurowski groggily found himself being wheeled to hospital room 666 to recover from having a kidney removed. It was the mid ’90s and his teenage kidney was deemed “underperforming.” It was only 1/10 the size of his other kidney, so his medical team decided that it was best to remove the organ, as individuals are able to lead active and healthy lives with one functioning kidney. 30-something years later, he finds himself in Stage IV kidney failure and in search of a living kidney donor.
“Since August of 2024 I have known that I should be looking for a transplant donor but have been unsuccessful this far,” Zurowski says.
“People can be on the wait list for a deceased donor for 5-7 years,” says Transplant Social Worker Lori Cragen, LICSW of The Transplant Center at RI Hospital. She is part of the Living Kidney Donor program, which is the only living kidney donor program in RI. “There are multiple benefits to a living donor. The surgery can be scheduled which means less wait time, there are better outcomes, lower risk of infection and lower doses in immunosuppressants. It essentially gets someone off the list sooner than later.”
Damaso Villanueva was born with an array of health issues, including only one kidney that was small and not functioning properly. Not expected to live past a year, he defied the odds with his can’t-quit strength. At seven years old, his kidney took a turn for the worse and was put on dialysis for 12 hours a day while trying to find a living donor. Ten potential donors were identified but all ruled out for various medical reasons, putting him on the wait list for a deceased donor.
“The process to approve a living donor was stricter than I had expected,” says his mother, Carla Longpre.
“Living donors need to be in overall good health (free from diabetes, uncontrolled blood pressure, obesity, cancer, chronic infection, etc),” Cragen says. “There is a thorough medical and psychiatric work up to make sure the living donor is a good candidate and up for surgery. The team decides that the person is healthy enough and will return to baseline health after recovery.”
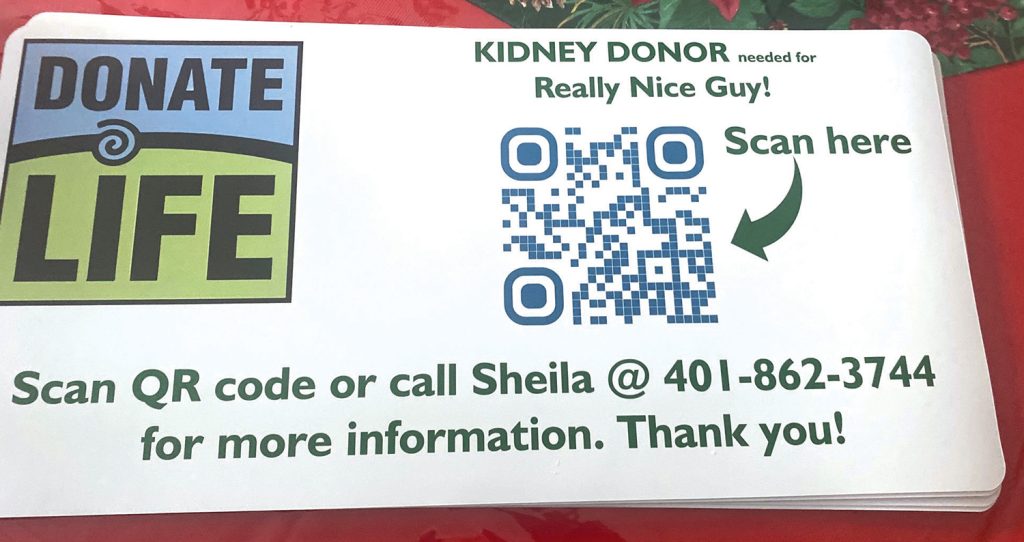
Zurowski has been methodically searching for a living donor. He first started using social media to tell his story in hopes that someone would volunteer and become a match. He requested people contact him or RI Hospital directly for more information on the process. Due to patient privacy, he will not know if anyone reached out unless they are deemed a match or the person contacted him directly.
“In the past several months I’ve seen this process pick up momentum to the point I’ve labeled it a true community project,” Zurowski says, adding that he is privileged to bring awareness to the living donor program. “It went from small groups of people who knew about it, to being published and having an opportunity to be on TV to talk about my ongoing situation.”
“It’s a big time commitment,” Cragen says of living donors. “There is a recovery period (up to 12 weeks out of work depending on the job). There is physical activity and restrictions after the surgery. It should not change your lifestyle or your life expectancy in any way once recovered.”
“It’s important for donors to understand what their involvement and recovery period will be,” Zurowski says. “It’s also understanding that sacrifice is made for the purpose of helping someone to be able to get that second chance and resume their normal life after a transplant. It’s a heroic, unselfish act to become a donor, and you can also gain a new friend to forever be connected to.”
“We don’t discuss potential living donors with patients,” Cragen says. “All patients are HIPAA protected and have confidentiality. The teams have a weekly team meeting to discuss progress. We are all part of the larger interdisciplinary transplant program.”
Villanueva persevered through dialysis and multiple stays at Boston Children’s, including a month and a half for pancreatitis, as he and his family awaited the call that a suitable organ had been identified. He was removed from the list numerous times due to illness.
“It’s a waiting game,” Longpre says. “They can call you any time and you have 1-2 hrs to get to the hospital. When you get that call you are overwhelmed with emotions. Excited, scared, grateful, sad because someone lost their life. Our first call in May 2017 was all of those emotions. Once we arrived at the hospital we were admitted, per the plan. Our surgeon came in to speak with us after we arrived. He explained that he didn’t fully love the kidney once he inspected it himself and that he was going to reject it. There would be no transplant. We were devastated.”
Zurowski has felt the effects of his failing kidney. He doesn’t have the energy he once did and finds many activities taxing. He is not able to work full time, but manages to do what he can from home when he is up to the task. As a season ticket holder, he makes it a point to attend as many PC hockey games as possible and took a trip to Pittsburgh over the summer to visit with friends and attend a concert.
“I’ve seen the good side and the bad side of this process over time,” Zurowski says. “It’s been a lot of learning and patience. Experiencing disappointment is almost a given for anyone in the process until you find the right people who are supportive of the journey and want to help.”
Cragen says that a living kidney donation has an overall better outcome (expected 12-14 year lifespan) than an organ donor (expected 7-8 year lifespan). She notes that recipients report to feel better overall and no longer face the restraints of dialysis.
“People describe it as a second chance to have a better quality of life,” she says. “Many donors report emotional and spiritual growth after donating.”
It was another six months of waiting before Longpre got the call that there was a suitable kidney for her son. They rushed to Boston Children’s with optimism but fearing a repeat of their last experience. The kidney was deemed suitable and Villanueva was prepped for surgery as his mother headed for the waiting room.
“The surgery for the transplant is long,” Longpre says. “I was terrified while I waited. So much can go wrong. Once they come out, recovery is long. The scariest part for us was when the new kidney just would not produce urine. Typically this happens within the first 24 hours. We were on day 8 post-op and still no urine. At this point we were told if he doesn’t produce urine by 9am day 10, they would consider the transplant a failure due to rejection. In typical Damaso fashion, he waited until 9:45am, day 10, to open the floodgates!”
RI passed legislation H 6065/S 0829, which provides paid medical leave to full-time employees for the purpose of donating an organ or bone marrow. The bill provides paid medical leave for a maximum of 30 days for full-time employees. Governor Dan McKee signed the bill into law on July 1, 2025.
“The new law has caused some confusion,” Cragen says, noting that they’ve received many inquiries. “We talked to TDI for clarification and learned that there has not been a change in paid leave for individuals that pay into TDI. They can take up to 12 weeks of paid leave off if they’re a living kidney donor. Our understanding is that the new law “expands TCI to provide job protection for 30 days for organ donors.”
Zurowski reports that his medical team is available and informative. He says that it’s easy to reach out to any of them during the week whether it’s for questions, updating medical records or just checking in.
“Damaso’s quality of life has improved incredibly since he recovered from his transplant,” Longpre says. “For almost two years prior he was on dialysis (PD) and needed to be connected to a machine for 12 hours a day. Clearly that leads to a very restrictive lifestyle for the entire family. Prior to getting on dialysis the kidney function has to drop down to a certain percent of function. Damaso was very ill at that point and it was very difficult to watch, as a mom, or anyone that loves the recipient.”
While not on dialysis yet, Zurowski did have surgery to put a fistula in his left arm for when/if that time comes. He remains hopeful that he will find “his hero” and is grateful for the people this journey has introduced him to and/or grown closer with. He has educated himself through his own research or speaking with former donors. He has become an educator and advocate, hoping that his story will benefit others as he searches for a lifesaver.
“It’s okay to be upset and not be prepared to handle the massive amount of work to be done, but it can be done with the support of people around you,” Zurowski reassures. “Once I’ve finished up my part of the process, get the transplant, I’m open to being available to others who find themselves in need of someone to talk to if it would help. I may not have a spare kidney to give back, but I’ve gained plenty of knowledge through this process.”
RI has approximately 362 people awaiting a kidney transplant. Cragran reports that the living donor program currently has 29 donors in the process. She encourages interested parties to reach out at any time, noting that the team ensures they are fully prepared and that they can opt out at any time up until the final surgery prep.
“All calls are anonymous,” Cragen says. “We gather information and urge people to talk it over with loved ones and consider the commitment. We make sure that the donors are informed and comfortable with their decision to enrich someone’s life.”
“If you’re new to needing an organ transplant it can be scary and life changing in equal parts,” Zurowski says. It was scary for me doing part one of the clinic and hearing all this new information. I was very overwhelmed, but with the guidance of the transplant team in the hospital, the weight of this has been removed significantly.”
“I wish everyone would become knowledgeable on becoming a donor,” Longpre says. “There are many ways to become a donor, whether it’s donating while you are still alive or checking that ever so important box when you renew your license. There’s no bigger/better way to share yourself. I’m not sure how to appropriately thank a grieving family who lost their loved one but gave my loved one the gift of life. We are forever grateful for our donor, as I’m sure every recipient and family are!”
brownhealth.org/centers-services/transplant-center